Better imaging, fewer surgeries?
Ovarian cancer study will use innovative photoacoustic and ultrasound technology
Ovarian cancer is the fifth-leading cause of death among women in the U.S. Since there is no effective screening option, surgical removal of the ovaries is often performed if a suspicious ovarian mass is found or if a woman is thought to be at high risk based on family history or genetic predisposition. A team of engineers and physicians at Washington University in St. Louis plan to shape our understanding of the best timing in a woman's life to undergo these potentially life-saving surgeries, without detriment to quality of life.
With a five-year, $2.55 million, multi-investigator grant from the National Institutes of Health's National Cancer Institute, Quing Zhu, professor of biomedical engineering in the McKelvey School of Engineering, will work with a team of Washington University School of Medicine physicians, including Andrea Hagemann, MD, associate professor of obstetrics & gynecology; Cary Siegel, MD, professor of radiology; and Matthew Powell, MD, chief of the Division of Gynecologic Oncology and professor of obstetrics and gynecology; to add an imaging method to the current standard of care for women at high risk for ovarian cancer. Using an innovative combined photoacoustic and ultrasound technology (PAT/US) Zhu and her team developed, they will conduct a clinical study to determine whether the technology will better detect and determine whether an ovarian mass is cancerous or benign, therefore improving current clinical practice.
The study will include two groups of women: those at risk for ovarian cancer due to a suspicious ovarian mass or family history, as well as women who have a deleterious mutation of the ovarian cancer genes, for example, the BRCA1 and BRCA2 mutations, shown to have a high risk of breast and ovarian cancers. The standard of care for women at high risk for ovarian cancer had traditionally been regular transvaginal ultrasound every six months and blood tests for the cancer antigen CA 125. However, ultrasound is not very effective at identifying early-stage disease, and CA 125 is not specific because some patients who have ovarian cancer may not have increased CA 125 levels.
"Current standard of care for women with the BRCA1 and BRCA2 mutations is to have the ovaries removed between ages 35-45 because of the high risk of ovarian cancer," Zhu said. "So this is a very desperate group of women who really want to find a screening method that gives them the assurance that they don't have cancer. Most of them who have their fallopian tubes and ovaries removed at a younger age for risk-reduction find out they are normal or benign. We hope our technique can help individualize guidelines for risk-reduction surgeries to improve patient quality of life without sacrificing cancer detection."
Powell, one of the principal investigators of the study, said standard imaging is not effective at distinguishing benign cysts from cancerous cysts in the ovaries.
"There really is a need for new imaging," he said. "We've been looking at ultrasound screening for ovarian cancer for 30 years and have seen slight hints that it might be helpful. But the technology is not advanced enough, and the concern is that it has caused as much harm as it has helped because we have to operate on so many patients."
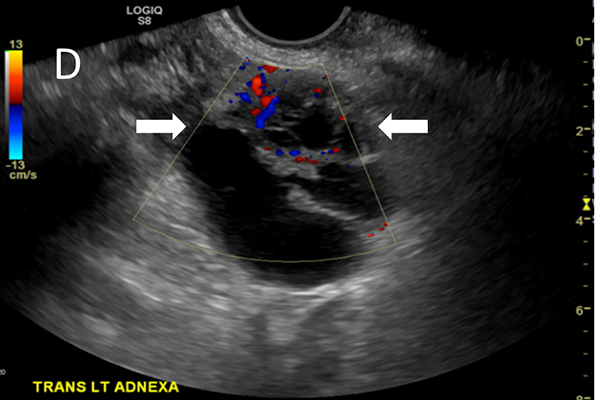
The study stems from positive results in a 2017-2018 pilot study when Zhu and the team tested the co-registered PAT/US. She and members of her lab created a sheath with optical fibers that wraps around a standard transvaginal ultrasound probe used to take images of ovaries suspected to be cancerous. The light from the laser propagates, gets absorbed by the tumor and generates sound waves, revealing information about the tumor vasculature and blood oxygen saturation (sO2) inside the ovaries made visible by the ultrasound. In the pilot study, the PAT/US technology identified invasive ovarian cancers based on higher levels of relative total hemoglobin (rHbT) and lower sO2 than benign and normal ovaries.
In the new study, Zhu and her team will use the PAT/US technology to get a detailed look at the blood vessels and sO2 in the ovaries of about 250 patients at the School of Medicine and Barnes-Jewish Hospital who are at risk for ovarian cancer or have the deleterious genetic mutation in one of the ovarian cancer genes. The team will enroll women who are within a few months of having surgery to remove their ovaries and high-risk women who have risk-reduction surgery within two years. For high-risk patients, the team will follow the patients every six months for up to two years to evaluate the ovarian lesion vasculature and sO2 changes to determine if the PAT/US can be used as an effective screening tool for early detection of ovarian cancer. The radiology and gynecology clinical trial offices will work together on patient recruiting and regulatory support.
"Our pilot study was well tolerated, and patients were very accepting of it," Powell said. "We can get the new technologies, but patients have to be willing to help other people. It may not affect how we treat them, but hopefully, it will affect patients in the future."
In addition, Zhu and her team plan to develop a machine-learning algorithm to recognize patterns, both benign and malignant.
"I hope that this technology will become one that helps these women and gives them some assurance with good accuracy that they can rely on," Zhu said. "It's very rewarding to see how an engineer developing technology can benefit a patient down the line."




