‘A leap forward’ in risk management of rectal cancer
Images from a probe, combined with deep learning, better differentiated residual cancerous tissue from recovered healthy tissue after chemoradiation treatment
Rectal cancer, along with colon cancer, is the third-most common type of cancer in the United States, and treatment and surgery greatly affect the quality of life of the patients. A multi-disciplinary team at Washington University in St. Louis has developed and tested an innovative imaging technique that is able to differentiate between rectal tissues with residual cancers and those without tumors after chemotherapy and radiation, which could one day help to avoid unnecessary surgeries in some patients who have achieved complete tumor destruction after chemoradiation.
Quing Zhu, professor of biomedical engineering in the McKelvey School of Engineering, and members of her lab developed a system using a new imaging technique — acoustic resolution photoacoustic microscopy co-registered with ultrasound (AR-PAM/US), paired with a “deep learning” artificial intelligence neural network — that was better able to determine the presence of residual tumors in treated rectal tumor bed tissues than other types of imaging, such as MRI, which is often unable to discern residual cancer from scar tissue. Results of the research — the first feasibility study using AR-PAM imaging in patients with rectal cancer previously treated with radiation and chemotherapy —are published in the journal Radiology March 23, 2021.
“Our PAM/US system paired with the deep learning neural network has great potential to better identify patients suitable for nonoperative management and improve patient quality of life,” Zhu said. “If we can tell after radiation and chemotherapy which patients may have a good response with no residual tumors, the patient may be able to avoid surgery.”
Zhu, also a professor of radiology at the School of Medicine, and doctoral students Xiandong Leng, co-first author on the paper with Shihab Uddin, who earned a doctorate in biomedical engineering from McKelvey Engineering in 2020; Hongbo Luo; and Sitai Kou, conducted a yearlong prospective study of patients with rectal cancer treated at Barnes-Jewish Hospital in St. Louis by School of Medicine clinicians Matthew Mutch, MD, the Solon and Bettie Gershman Chair in Colon and Rectal Surgery, chief of the Section of Colon and Rectal Surgery and professor of surgery; and William Chapman Jr., MD, a resident physician in surgery. Steven R. Hunt, MD, associate professor of surgery; Anup Shetty, MD, assistant professor of radiology; and Deyali Chatterjee, MD, assistant professor of pathology & immunology; and Michelle Cusumano, study coordinator in the Section of Colon and Rectal Surgery, also significantly contributed to the study, Zhu said.
Current treatment calls to remove the rectal tissue when there is uncertainty about a diagnosis, which leads to surgeries performed on patients with no active cancer, Chapman said. Side effects of the surgery can include wound complications, chronic pain and permanent colostomies in about 30% of patients. Patients who don’t have surgery must have quarterly invasive exams since the current imaging sensitivity is poor.
Chapman said the team had spent more than three years investigating this technology in surgically-removed colon and rectum specimens with promising results before developing the prototype for patient studies.
“We hope that improved imaging provided by AR/PAM will significantly improve our ability to discriminate between patients with residual tumor and those who have been completely cured without surgery,” he said. “By both avoiding morbid, unneeded surgery and reducing the burden of surveillance testing, photoacoustic imaging could be a leap forward in the current management of locally invasive rectal cancer.”
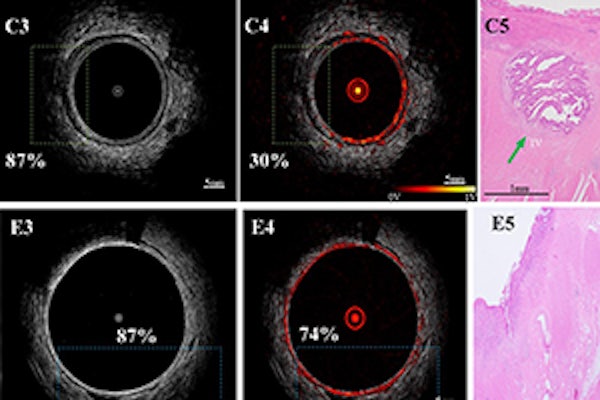
In the study, after completing chemotherapy and radiation, patients underwent PAM/US imaging with a handheld endorectal laser probe developed in Zhu’s lab. The probe has a rotating head that allows for a 360-degree image of the rectum, the last 6 inches of the colon. The end of the probe, which takes one image per second, is covered by a small latex balloon that is inflated with water that allows transmission of the ultrasound and photoacoustic waves to the rectal wall. These waves highlight changes in the vasculature in the tissue and as well as new tumor growth. The imaging procedure added about 20 minutes of time that patients were under anesthesia.
Leng, who has been working on this project since 2017, was instrumental in system and software development, Zhu said. He designed and built the AR/PAM endoscope — the first of its kind — and programmed the system to acquire data and process and display images in real time.
“From the very preliminary ex vivo data, my setup clearly disclosed multi-layer structure from ultrasound image and rich blood vessels in the submucosa of normal colorectal tissue,” Leng said. “In contrast to normal tissue, malignant tumor bed shows a lack of multilayer structure and blood vessels. This important finding may reveal an important feature accessing patients’ treatment response to chemotherapy and radiation therapy.”
In the first phase of the study, the team used data from surgically-removed tissue specimens from more than 2,000 images from 22 patients to train the neural network, an artificial intelligence-based set of algorithms that operates similar to the human brain, to recognize normal and cancerous colorectal tissue. In the second phase, they used images from the living tissue from 10 patients who had previously undergone chemotherapy and radiation. Several hundred images from five of those patients were used to fine-tune the neural network, and hundreds of images from five patients were withheld for testing.
The deep-learning PAM model, designed and developed by Uddin, correctly predicted the cancerous status of all five of the patients who had undergone imaging, while the MRI images misclassified three out of five patients, and ultrasound-only deep-learning model incorrectly declared three patients as cancer-free.
Mutch said the team is very optimistic about the results.
“This is spectacular news, and it moves us closer in the transition from concept to clinically-useful technology,” he said. “The hope is that it will allow us to differentiate patients who had a complete response to chemotherapy and radiation from those patients with residual tumor. This will help better determine which patients can be managed nonoperatively versus those who truly need an operation.”
Going forward, the team plans to conduct a clinical study to confirm these initial results in a large group of rectal cancer patients who have completed chemotherapy and radiation and will undergo surgery or follow patients after treatment.
Leng X, Shihab Uddin K M, Chapman Jr. W, Luo H, Kou S, Amidi E, Yang G, Chatterjee D, Shetty A, Hunt S, Mutch M, Zhu Q. Assessing rectal cancer treatment response using co-registered endorectal photoacoustic and ultrasound imaging. Radiology, March 23, 2021. https://doi.org/10.1148/radiol.2021202208
Funding for this research was provided by pre-R01 funding from the Siteman Cancer Center and the Foundation for Barnes-Jewish Hospital; and the National Cancer Institute R01CA237664.







