Multi-scale imaging technique may enable objective assessment of myofascial pain
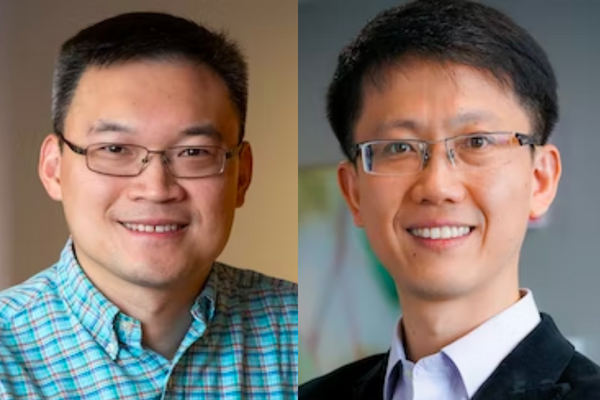
Song Hu, Yong Wang team up to find quantitative biomarkers for clinical pain management
About 50 million Americans experience chronic pain. For many, the pain involves the muscle and the fascia surrounding it, creating myofascial pain with trigger points. This chronic pain syndrome significantly affects patients’ daily functioning and quality of life. While there are treatments, including physical therapy, nonopioid or opioid medications and trigger point injections, adequately controlling this pain is challenging due to the lack of objective and quantitative pain biomarkers.
Song Hu and Yong Wang, both researchers at Washington University in St. Louis, plan to develop a set of novel imaging biomarkers of myofascial pain with a first-phase, three-year, $2.3 million technology development and observational clinical study grant from the National Center for Complementary & Integrative Health of the National Institutes of Health as part of the Helping to End Addiction Long-term (HEAL) Initiative, which provides funding for researchers to address opioid misuse.
Hu, associate professor of biomedical engineering in the McKelvey School of Engineering, and Wang, associate professor of obstetrics and gynecology in the School of Medicine and of electrical & systems engineering in McKelvey Engineering, expect that these biomarkers, which can be assessed at both the local trigger point and throughout the muscle tissue, would guide choices of appropriate pain management and ultimately reduce opioid misuse or addiction. In 2019, more than 70% of all drug overdose deaths were associated with opioids.
Hu and Wang will combine their expertise in imaging technology — Hu bringing fiber-optic imaging and sensing, and Wang bringing MRI and surface electromyography — to obtain the objective biomarkers, including muscle structure, stiffness, oxygenation, blood flow, metabolism and electrical activity, in three states: healthy, latent pain and active pain.
“We need two types of technology to provide a comprehensive assessment of the myofascial unit at different spatial and temporal scales,” said Hu, an expert in high-resolution photoacoustic and optical imaging. “These imaging techniques are highly complementary in providing a focal view at the microscopic level at the trigger point and a global view at the macroscopic level across the entire muscle in the human body.”
The fiber-optic technique to be developed in Hu’s lab will create a first-of-its-kind, hair-thin device that can be advanced through the needle used to inject pain-relieving drugs into the trigger point — providing microscopic, quantitative measurements at the trigger point.
“By going through the needle track, you break through the penetration limitation of light microscopy and can get internal imaging without causing additional invasiveness,” Hu said. “We can insert the fiber to provide localized trigger point measurement of the fine details, such as muscle fiber microstructure, microvascular perfusion, oxygenation, metabolism and stiffness.”
The MRI and electromyography techniques, which are Wang’s expertise, can comprehensively and noninvasively assess muscle physiology and pathology at the macroscopic level.
“MRI will image and quantify the muscle injury and edema, stiffness and oxygenation across the entire muscle before and after the drug injection,” Wang said. “Moreover, the surface electromyography system is wearable, portable and can be used to monitor electrical activities over the entire muscle repeatedly and continuously before, during and after the trigger point injection with high temporal and spatial resolutions.”
Hu and Wang have a team of Washington University collaborators, including Philip Bayly, the Lee Hunter Distinguished Professor and chair of the Department of Mechanical Engineering & Materials Science; Hongyu An, director of the Biomedical MR Center at Washington University School of Medicine’s Mallinckrodt Institute of Radiology and professor of radiology and of neurology in the School of Medicine and of biomedical engineering in McKelvey Engineering; Jie Zheng, associate professor of radiology at the Mallinckrodt Institute of Radiology; Yu-Qing Cao, associate professor of anesthesiology in the School of Medicine; Xiaobin Yi, MD, professor of anesthesiology at the School of Medicine and director of pain medicine at Missouri Baptist Medical Center; Ken Schechtman, professor of biostatistics in the School of Medicine; Peinan Zhao, assistant professor of obstetrics and gynecology in the School of Medicine; Stephanie Pizzella, clinical research supervisor; and Madison Copeland, clinical research coordinator.
After developing the technology and reaching the first-phase milestones, the imaging team led by Hu and Wang and the clinical pain management team led by Yi will have the opportunity to proceed to the second phase, which includes a two-year, $2.4 million clinical trial study on patients with various states of myofascial pain to test the efficacy of the imaging biomarkers for monitoring treatment responses and predicting clinical outcomes.




