New technology offers pathways to finding treatments for kidney disease
McKelvey Engineering, School of Medicine collaborate to develop hydrogel system
Chronic kidney disease and eventual kidney failure are incurable diseases that affect 13% of the U.S. population, particularly those with high blood pressure and diabetes. These diseases degrade the “podocyte” cells of the kidney that maintain the body’s blood filtration system, eventually sending patients to dialysis.
The search for effective treatments has been hampered because these highly structured cells cannot be cultured outside of the body, and because immortalized cell lines are not true to their structure. New research from Washington University’s McKelvey School of Engineering and the School of Medicine aims to overcome this critical barrier.
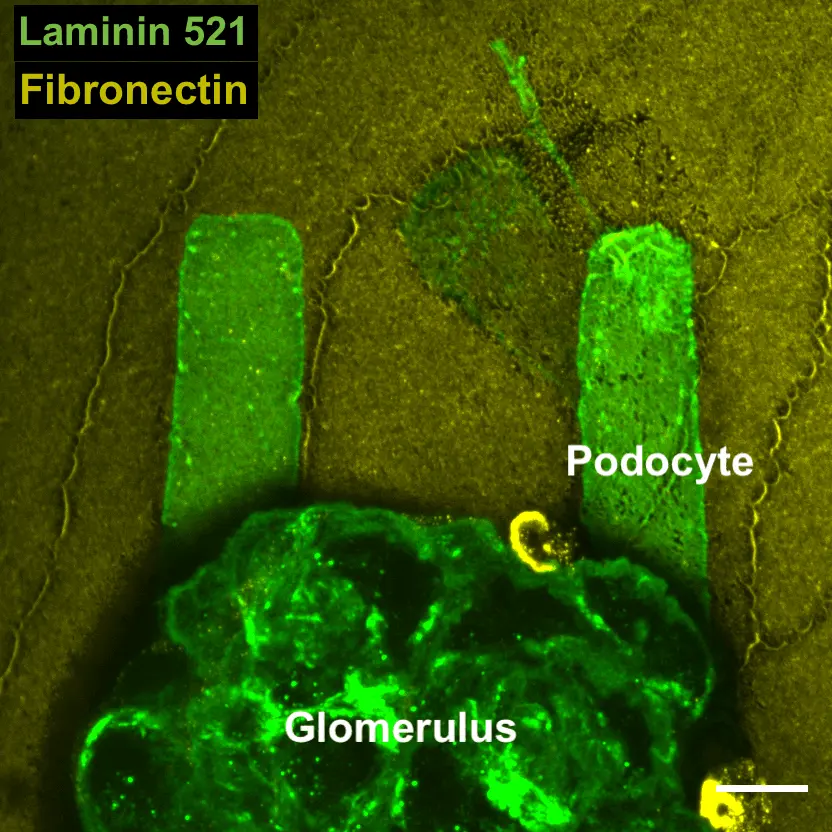
The discovery, published Aug. 31 in Science Advances, is enabled by a new hydrogel system that preserves the biochemistry and mechanical environments of cultured podocyte cells. With this system, podocytes taken from isolated glomeruli, the filtering units of the kidney, can be cultured on patterns of the proteins that would be in their vicinity in healthy and diseased kidneys. The cells rapidly adopt new shapes and express new protein structures that are associated with injury, enabling researchers to identify new ways to possibly control the mechanisms that these cells use to heal themselves.
“We now have a window into the cytoskeletal dynamics that underlie shape changes and cell loss in injury and disease,” said Hani Y. Suleiman, MD, PhD, assistant professor of medicine in the Division of Nephrology in the Department of Medicine at the School of Medicine and one of three senior authors of the study. “Our studies reveal the structure and function of wound-healing protein complexes that might serve as drug targets.”
Shumeng Jiang, a doctoral student in mechanical engineering & materials science, was first author in collaboration with the labs of senior authors Jeffrey Miner, the Eduardo and Judith Slatopolsky Professor of Medicine in Nephrology in the School of Medicine, and Guy Genin, the Harold and Kathleen Faught Professor of Mechanical Engineering in McKelvey Engineering.
Podocytes are unique cells with a hierarchical structure that includes almost octopus-like tentacles that form the structure for the kidney’s filtering units. Diseases that affect podocytes, such as diabetic nephropathy, disrupt these structures and lead to kidney failure that requires dialysis or transplantation.
“We have never before been able to see how these structures respond to stresses in real time,” Miner said. “The immortalized podocyte cell lines that we and others use do not develop these structures, and watching them inside a mouse is difficult. This new approach allows us to determine how mouse and human podocytes taken directly from kidneys behave in the laboratory, where they can be subjected to endless experimental conditions.”
“An exciting new angle is the ability to study and manipulate the mechanobiological aspects of cell responses to disease,” said Genin, who co-directs the National Science Foundation Science and Technology Center for Engineering Mechanobiology (CEMB). “We can now quantify how changes to the kidney associated with diabetes and elevated blood sugar affect the mechanical function of podocytes and their ability to recover.”
Washington University has submitted a patent application on the technology in cooperation with the university’s Office of Technology Management, and the team hopes to enable a range of research and eventually therapies using the system. Suleiman said he believes this technology has potential to transform development of therapeutics.
“Now that we can perform tests on human cells that come from diseased kidneys, we can rapidly screen chemical treatments that affect protein dynamics and mechanobiology and start to step toward treatments for a whole range of currently incurable diseases,” Suleiman said.
Jiang S, Alisafaei F, Yuan H, Peng X, Huang Y-Y, Miner JH, Genin GM, Suleiman HY. An ex vivo culture model of kidney podocyte injury reveals mechanosensitive, synaptopodin-templating, sarcomere-like structures. Science Advances, Aug. 31, 2022. https://www.science.org/doi/10.1126/sciadv.abn6027
This work was supported by the Washington University in St. Louis Office of the Provost; the National Institutes of Health (P30DK020579, R01DK131177, R01DK058366, R01DK078314, and R01DK128660); and the National Science Foundation (CMMI 1548571).