Air monitor can detect COVID-19 virus variants in about 5 minutes
Proof-of-concept device could also monitor for flu, RSV, other respiratory viruses
Now that the emergency phase of the COVID-19 pandemic has ended, scientists are looking at ways to surveil indoor environments in real time for viruses. By combining recent advances in aerosol sampling technology and an ultrasensitive biosensing technique, researchers at Washington University in St. Louis have created a real-time monitor that can detect any of the SARS-CoV-2 virus variants in a room in about 5 minutes.
The inexpensive, proof-of-concept device could be used in hospitals and health care facilities, schools and public places to help detect CoV-2 and potentially monitor for other respiratory virus aerosols, such as influenza and respiratory syncytial virus (RSV). Results of their work on the monitor, which they say is the most sensitive detector available, are published in Nature Communications July 10, 2023.
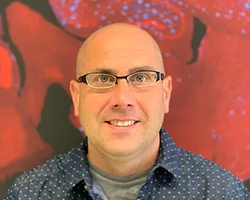
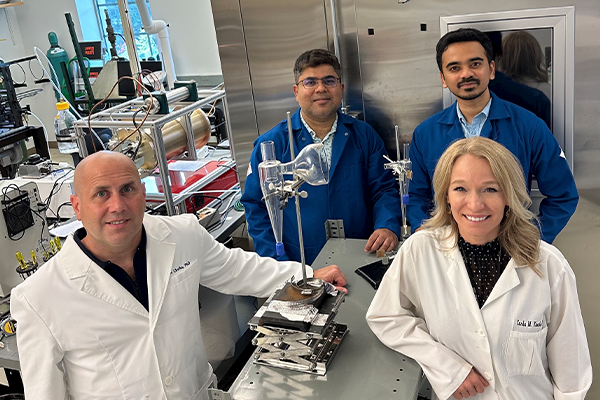
The interdisciplinary team of researchers from the McKelvey School of Engineering and the School of Medicine consists of Rajan Chakrabarty, the Harold D. Jolley Career Development Associate Professor of energy, environmental & chemical engineering in McKelvey Engineering; Joseph Puthussery, a postdoctoral research associate in Chakrabarty’s lab; John Cirrito, professor of neurology; and Carla Yuede, associate professor of psychiatry, both at the School of Medicine.
“There is nothing at the moment that tells us how safe a room is,” Cirrito said. “If you are in a room with 100 people, you don’t want to find out five days later whether you could be sick or not. The idea with this device is that you can know essentially in real time, or every 5 minutes, if there is a live virus.”
Cirrito and Yuede had previously developed a micro-immunoelectrode (MIE) biosensor that detects amyloid beta as a biomarker for Alzheimer’s disease and wondered if could be converted into a detector for SARS-CoV-2. They reached out to Chakrabarty, who assembled a team that included Puthussery, who had expertise in building real-time instruments to measure the toxicity of air.
To convert the biosensor from detecting amyloid beta to coronavirus, the researchers exchanged the antibody that recognizes amyloid beta for a nanobody from llamas that recognizes the spike protein from the SARS-CoV-2 virus. David Brody, MD, PhD, a former faculty member in the Department of Neurology at the School of Medicine and an author on the paper, developed the nanobody in his lab at the National Institutes of Health. The nanobody is small, easy to reproduce and modify and inexpensive to make, the researchers said.
“The nanobody-based electrochemical approach is faster at detecting the virus because it doesn’t need a reagent or a lot of processing steps,” Yuede said. “SARS-CoV-2 binds to the nanobodies on the surface, and we can induce oxidation of tyrosines on the surface of the virus using a technique called square wave voltammetry to get a measurement of the amount of virus in the sample.”
Chakrabarty and Puthussery integrated the biosensor into an air sampler that operates based on the wet cyclone technology. Air enters the sampler at very high velocities and gets mixed centrifugally with the fluid that lines the walls of the sampler to create a surface vortex, thereby trapping the virus aerosols. The wet cyclone sampler has an automated pump that collects the fluid and sends it to the biosensor for seamless detection of the virus using electrochemistry.
“The challenge with airborne aerosol detectors is that the level of virus in the indoor air is so diluted that it even pushes toward the limit of detection of polymerase chain reaction (PCR) and is like finding a needle in a haystack,” Chakrabarty said. “The high virus recovery by the wet cyclone can be attributed to its extremely high flow rate, which allows it to sample a larger volume of air over a 5-minute sample collection compared with commercially available samplers.”
Most commercial bioaerosol samplers operate at relatively low flow rates, Puthussery said, while the team’s monitor has a flow rate of about 1,000 liters per minute, making it one of the highest flow-rate devices available. It is also compact at about 1 foot wide and 10 inches tall and lights up when a virus is detected, alerting administrators to increase airflow or circulation in the room.
The team tested the monitor in the apartments of two COVID-positive patients. The real-time PCR results of air samples from the bedrooms were compared with air samples collected from a virus-free control room. The devices detected RNA of the virus in the air samples from the bedrooms but did not detect any in the control air samples.
In laboratory experiments that aerosolized SARS-CoV-2 into a room-sized chamber, the wet cyclone and biosensor were able to detect varying levels of airborne virus concentrations after only a few minutes of sampling.
“We are starting with SARS-COV-2, but there are plans to also measure influenza, RSV, rhinovirus and other top pathogens that routinely infect people,” Cirrito said. “In a hospital setting, the monitor could be used to measure for staph or strep, which cause all kinds of complications for patients. This could really have a major impact on people’s health.”
The team is working to commercialize the air quality monitor.
Puthussery JV, Ghumra DP, McBrearty KR, Doherty BM, Sumlin BJ, Sarabandi A, Mandal AG, Shetty NJ, Gardiner WD, Magrecki JP, Brody DL, Esparza TJ, Bricker TL, Boon ACM, Yuede CM, Cirrito JR, Chakrabarty RK. Real-time environmental surveillance of SARS-CoV-2 aerosols. Nature Communications, July 10, 2023. Doi: 10.1038/s41467-023-39419-z
This research was funded by the National Institutes of Health (NIH) RADx-Rad program (U01 AA029331, U01 AA029331-S1); NIH National Institute of Neurological Disorders and Stroke Intramural Research Program, SARS-CoV-2 Assessment of Viral Evolution (SAVE) Program; and WashU-IITB Joint Master’s Program.