Wearable tech for contact tracing joins fight against COVID, future pandemics in hospitals
An interdisciplinary team including Chenyang Lu and M Cristina Vazquez Guillamet has developed CATCH, a potentially powerful automated tool for mitigating the spread of infectious diseases among frontline health care workers
In the battle against COVID-19, contact tracing has proven to be a vital weapon in curbing the spread of the virus. While numerous contact tracing methods have emerged, manual contact tracing methods are often slow and inaccurate while smartphone-based tracing suffers low adoption rates, due in part to privacy concerns. Furthermore, these solutions do not work effectively for health care workers at high risk for infections.
To address these limitations, researchers led by Chenyang Lu, the Fullgraf Professor in the McKelvey School of Engineering and director of the AI for Health Institute at Washington University in St. Louis, have developed Contact Tracing for Hospitals (CATCH), an automated contact tracing system designed specifically for the unique challenges and risks faced by frontline health care workers in the hospital environment. The work was published Sept. 27 in Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies and presented Oct. 10 at the UbiComp conference in Cancún, Mexico.
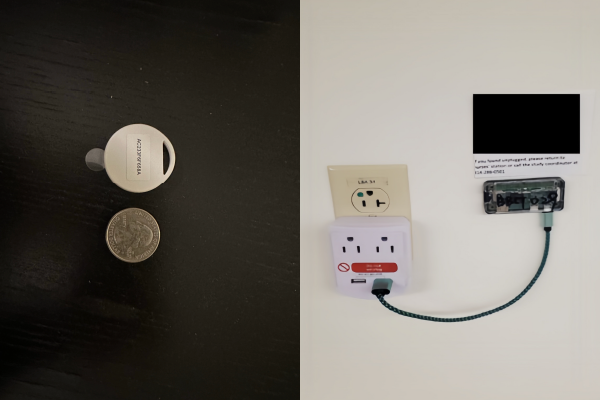
CATCH’s creative design allows it to be deceptively simple yet highly effective. Health care professionals in the intensive care unit attach a coin-sized Bluetooth low energy (BLE) beacon to their badges. These beacons transmit signals to strategically placed anchors, small receivers plugged in around the ICU, which in turn securely store the information on a server where it can be queried for a contact tracing report if someone tests positive.
The BLE beacons address privacy concerns – the beacons’ signals are emitted and captured only in the intensive care unit – and allow health care professionals to avoid cellphone-based tracking.
“Based on discussions with health care professionals, we recognized the diversity in environmental characteristics and working patterns and were inspired to explore the possibility of employing distinct contact tracing methods tailored to different room types,” said Jingwen Zhang, first author on the paper and a graduate student in Lu’s lab. “For instance, one notable hotspot for close contacts within the ICU is during morning rounds when a group of health care workers collaboratively discusses patients in the hallway, which typically lasts for several hours. To deal with this close contact scenario, our contact tracing system incorporated a customized clustering contact tracing method designed to identify members of the patient round team accurately.”
By customizing CATCH to suit the environmental characteristics and health care worker behaviors in different areas of the ICU, the team developed a more accurate and efficient system for identifying close contacts. CATCH employs a suite of novel contact tracing algorithms tailored for each scenario. This approach ensures that CATCH can adapt to the complex dynamics of a hospital environment to achieve superior accuracy in contact tracing compared to existing approaches.
The researchers evaluated CATCH’s real-world usability in the COVID-19 ICU of Barnes-Jewish Hospital, where CATCH consistently outperformed other contact tracing approaches in terms of accuracy, effectiveness and efficiency.
“When we simulated positive cases, the CATCH system had an additional contact yield of 15% and would decrease the effective reproduction number, a measure of viral spread, by more than half,” said Maria Cristina Vazquez Guillamet, MD, an associate professor of medicine in the Division of Infectious Diseases at Washington University School of Medicine. “This would ultimately lead to significantly less transmission between health care workers. Our system can easily be scaled up and its parameters reconfigured so it can be deployed in any viral outbreak.”
By swiftly identifying and isolating potential COVID-19 exposures – returning a highly accurate list of contacts in just 20 minutes – CATCH can reduce the risk of virus transmission within hospital units, ultimately saving lives.
“The great strengths of CATCH are that it is automated and highly flexible, making it a powerful tool in pandemic preparedness now and in the future,” Lu said. “CATCH can be easily tailored in its parameters, then automatically carry out effective contact tracing in a wide range of scenarios. For example, COVID-19 close contacts are defined as being within six feet for at least 15 minutes over a 24-hour period, but the next pathogen could be different. We can change those settings in CATCH and easily reuse the system for the next pandemic.”
Zhang J, Dai R, Rjob A, Wang R, Hamauon R, Candell J, Bailey T, Fraser VJ, Vazquez Guillamet MC, Lu C. Contact tracing for health care workers in an intensive care unit. Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies, 7(3), Article 141, Sept. 27, 2023. DOI: https://doi.org/10.1145/3610924
This research was supported by CDC Broad Agency Announcement awards (BAA) 75D301-20-R-68024; CDC epicenter grant U54CK000609; the National Institutes of Health (NIH) Clinical and Translational Science Awards (CTSA) UL1TR002345; and the Fullgraf Foundation.





